 Get a demo
Get a demo Get a demo
Get a demo
Oncology practices throughout the U.S. are too busy diagnosing & treating cancer to waste a second, and yet claim issues, delayed patient payment, and the tight margins for high-dollar treatments wage an unrelenting battle on your revenue cycle team.
Ongoing treatment makes precollection necessary & difficult to assess
No system to check if billed amounts exceed prior authorization
Fear & stress make patient communication extremely sensitive
High dollar drugs with changing unit measurements make backend claim issues inevitable & hard to rework
Payer contracts have difficult payment intricacies

Rivet levels the "paying field" for oncology practices looking to collect more – faster — and more accurately from patients and payers. With Rivet as your oncology revenue cycle sidekick, you can:
Automate accurate patient cost estimates & precollection
Streamline communication for patients to understand expectations & costs
Audit claims in seconds to reveal systemic payer issues & provide proof to insurers for denials & underpayments
Evaluate payer contract change needs through modeling & comparison
Accurately forecast revenue through claim auditing & evaluation


Take an in-depth look at the most common underpayment projects within your revenue cycle.
Download now
Use new payer data to boost your negotiations.
Download now
Get more out of your commercial payer contracts.
Download now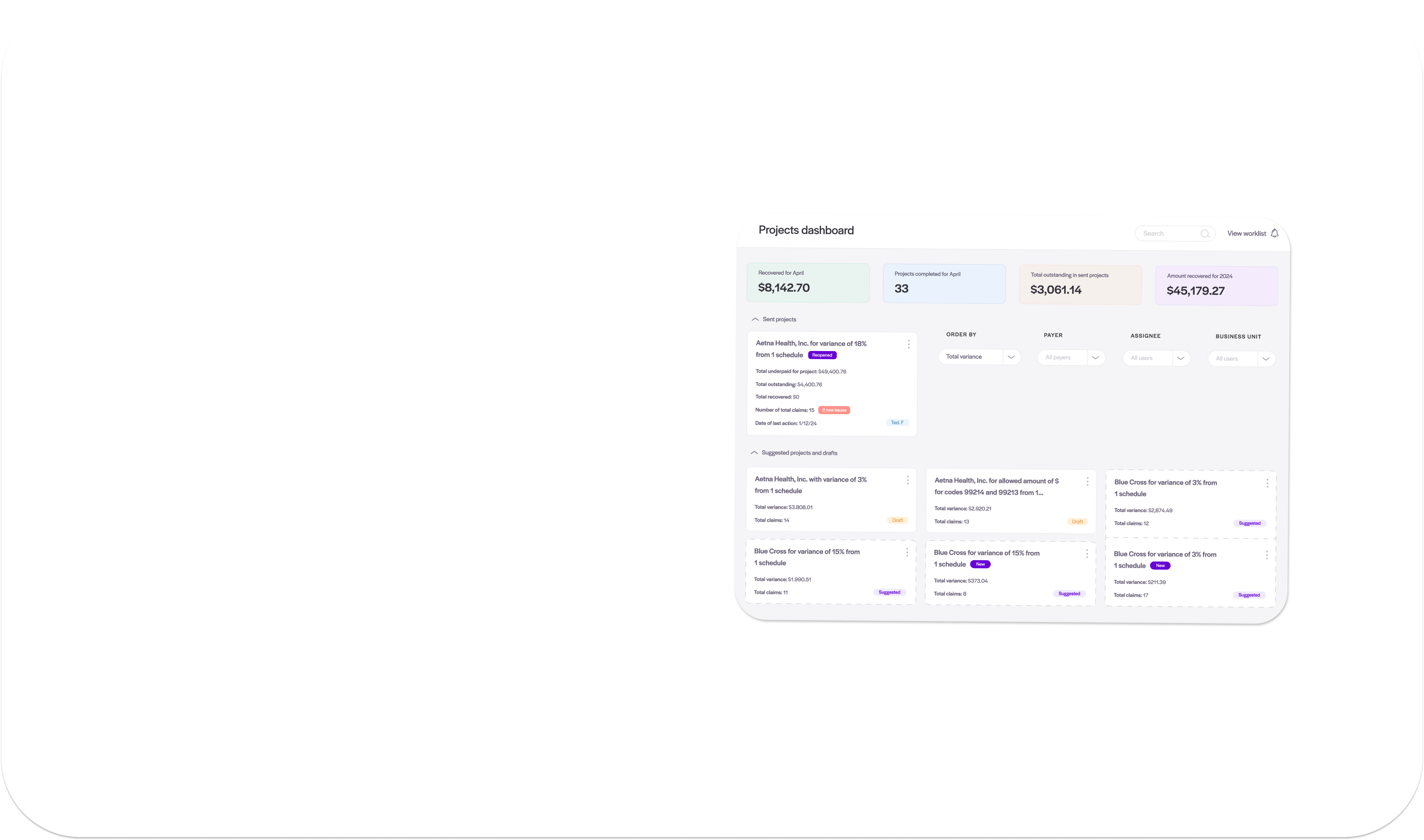
Your revenue backbone for accurate reimbursement — fast.
- Establish an easy to maintain payer contract management platform
- Benchmark rates & model scenarios for negotiations
- Auto-detect & solve for underpayments

Explore practical methods for predicting revenue.
Download now
Financial experts break down net revenue forecasting.
Watch on demand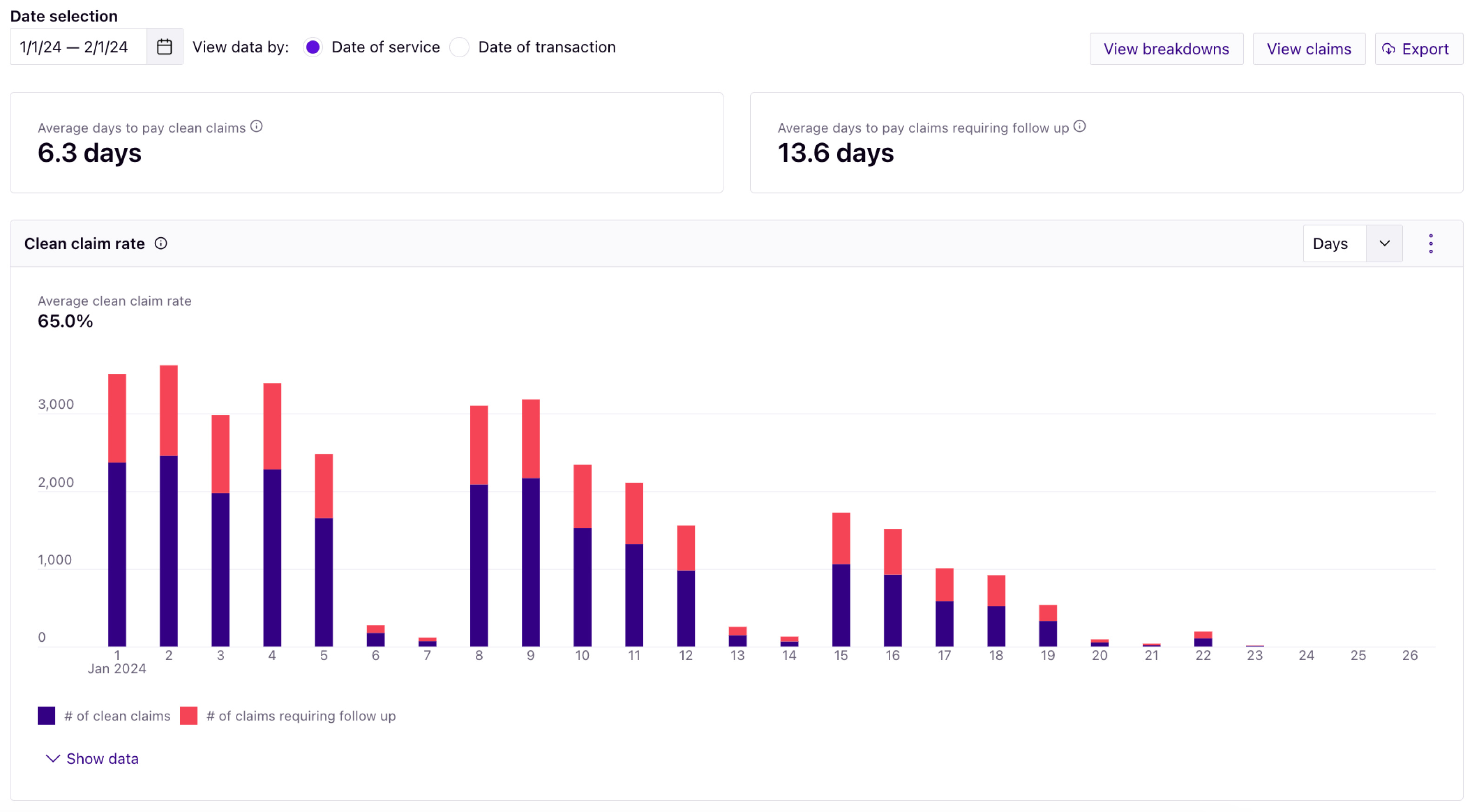
Take advantage of growth opportunities.
Watch on-demand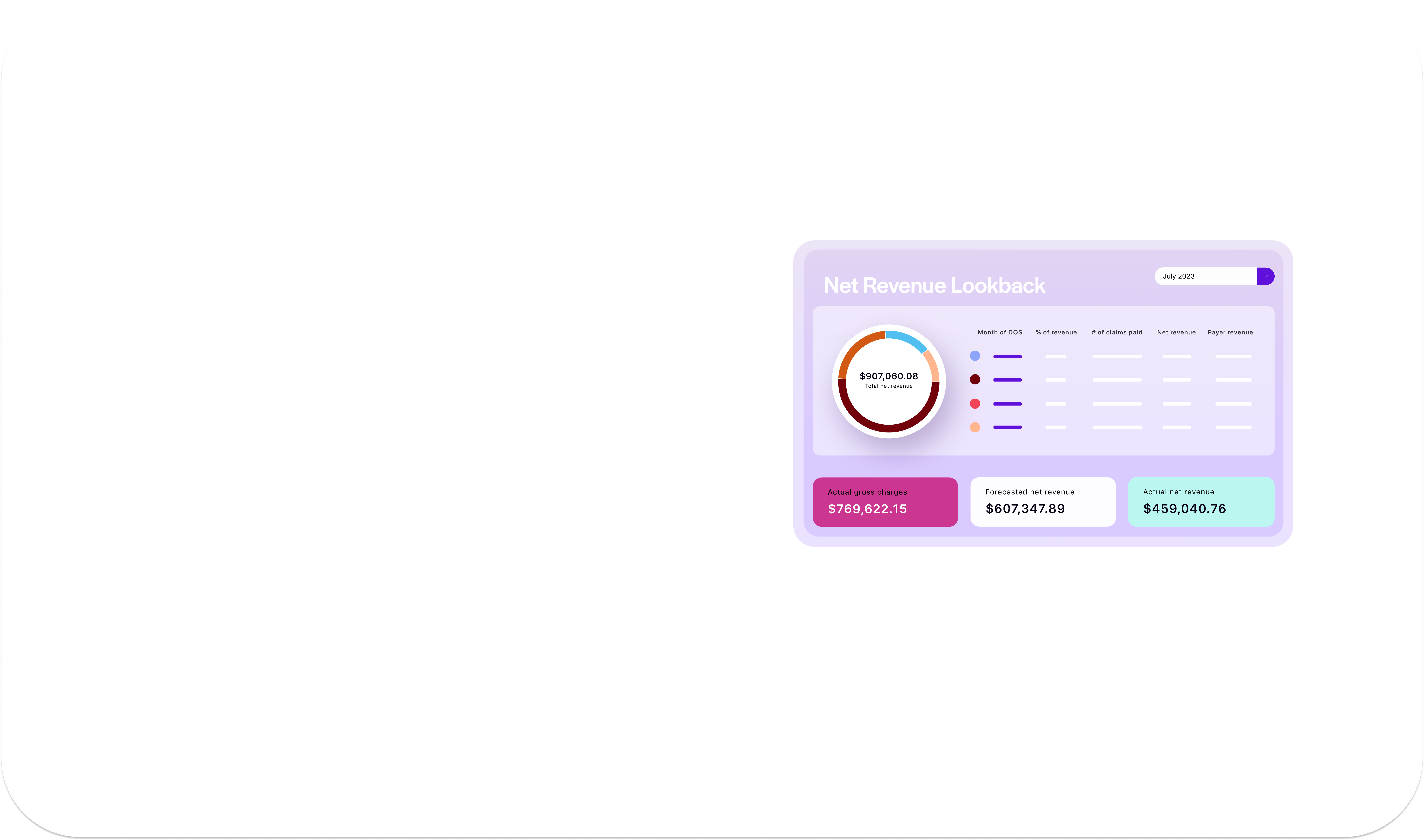
Take your claims insights to a whole new level.
- Analyze data for your payers, adjudication cycles, denials, and so much more
- Prevent and rework denials with easy-to-use billing edit suggestions
- Model revenue predictions in seconds

What is the secret to collecting more patient responsibility from your patients?
Collect at the right time.

Address critical workflow considerations to align cash targets based on seasonality.
Watch on demand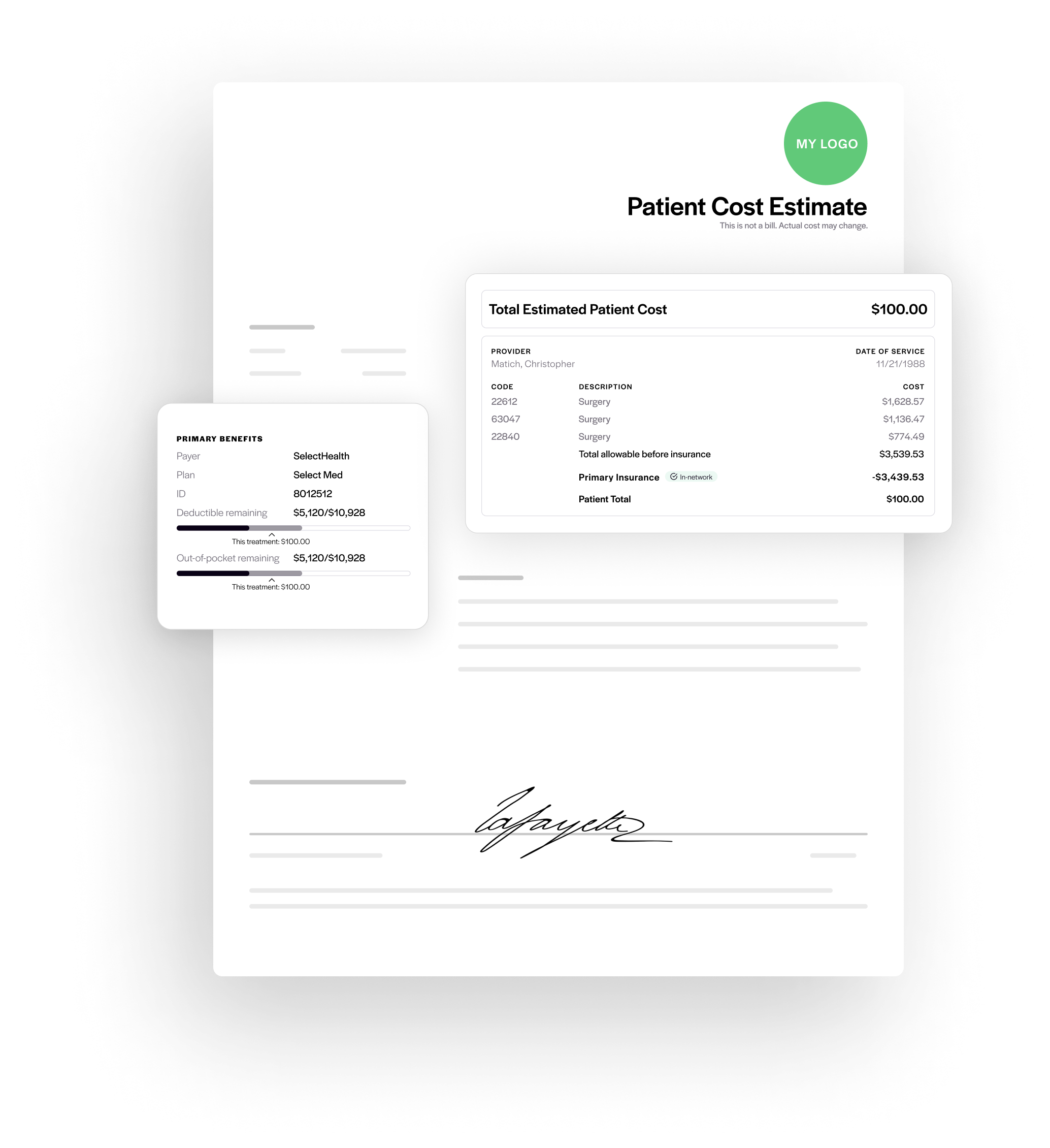
Shift the patient financial experience to maximize revenue.
Watch on demand
Automated, accurate patient Good Faith Estimates in seconds.
- Deliver real-time eligibility, in-network and out-of-network benefits
- Provide accurate deductible & OOP balances remaining
- Secure payment through email & SMS options
Shine a light on how to decrease denials and rescue revenue.
Download now
Increase productivity to capture missed revenue.
Watch on demand
You’re leaving money on the table.
Watch on demand
Recover every denial in
record time.
- Gain denied and non-response claim dashboards, worklists, and team assignments
- Store instruction and best practice documentation
- Breakdown denial reasons by group and individual claims

