Free On-Demand Webinar
Take a deep dive into the techniques payers use to short you and how to combat those issues while contracts are in effect.

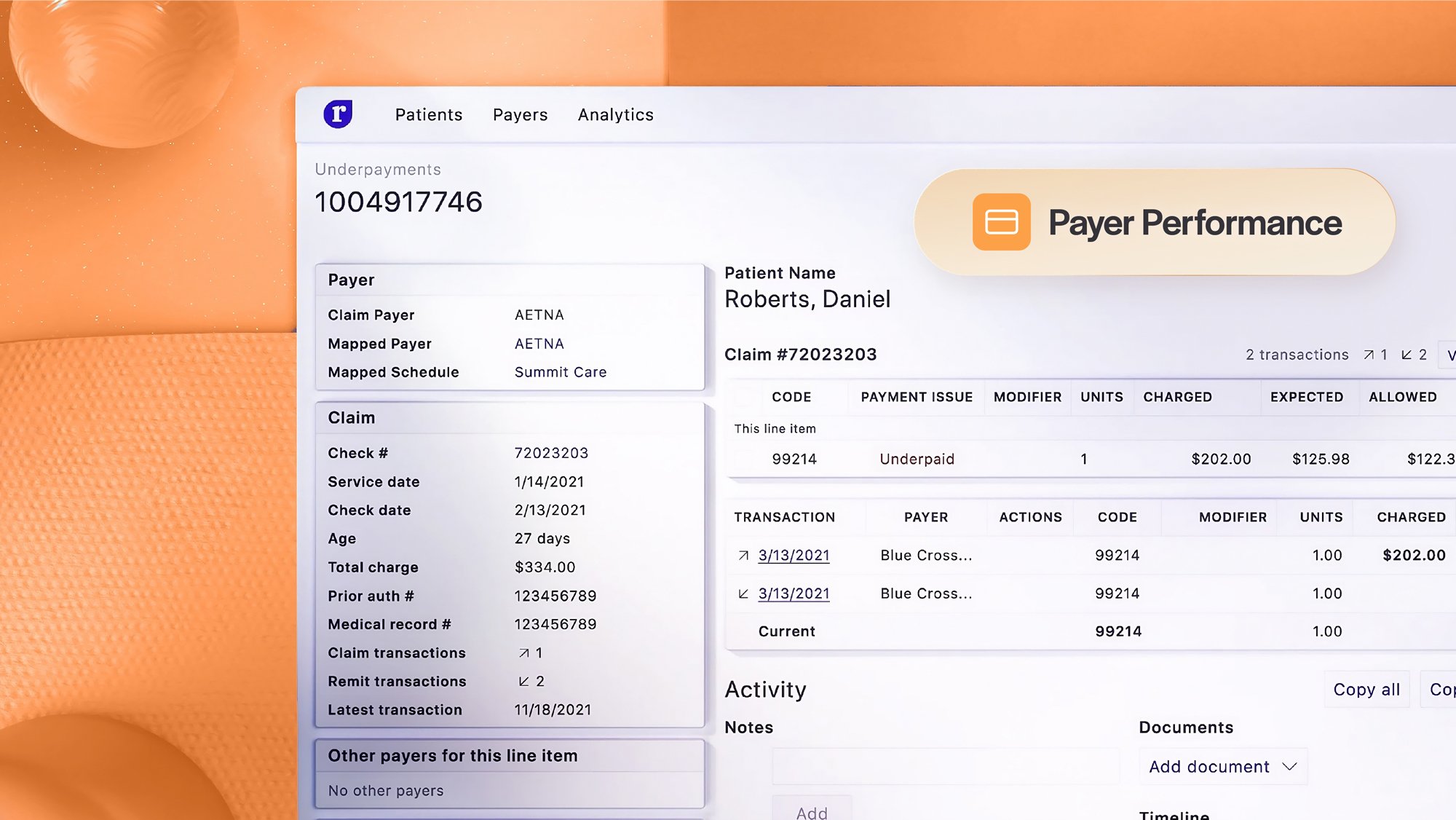
The Medical Group Management Association (MGMA) approximates that insurers routinely underpay U.S. healthcare providers by 7–11%. Your payers are underpaying your contracted rates, denying claims, and using your contracts themselves to keep you from being paid what you deserve.
In our upcoming webinar, we’ll explore the following topics about what in your contracts could be keeping your organization from appropriate payment:



